I haven’t written in a bit, and I owe you the truth.
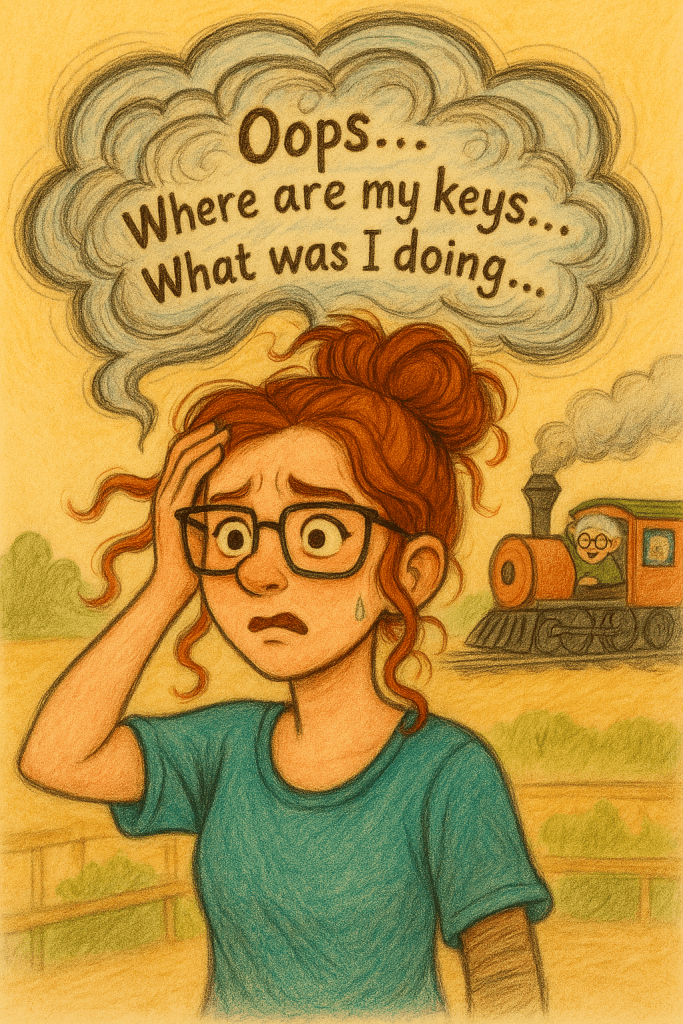
It’s not because I ran out of stories. It’s because I got mired in the muck—same as each of you. Sometimes I have to step back and manage my own brain before I can put words on a page that are worth reading. Caregiving has a way of swallowing your bandwidth whole. One minute you’re fine-ish, and the next you’re standing in the kitchen trying to remember if you fed the dog, took your vitamins, or brushed your teeth… and honestly, it could be none of the above.
You know the drill. The lost identity. The constant low-grade worry. Trying to find balance between cooking, cleaning, keeping someone safe, keeping yourself sane, and figuring out how to squeeze out even fifteen minutes where you can just… live. And then the rare time you do grab a little oxygen for yourself, there’s judgment.
Yes. The Karens are alive and well! They’re out there in the wild. They don’t know your situation (and they probably have their own), but they sure do have opinions about it and your life and what you “should” be doing. Trust me, when I say, that when we get to Heaven God is going to be talking to them about them, not about us. Let the self righteousness, high and mighty, roll off your back like water off a duck. Most of the time, I can, but recently, I haven’t been able to let it go so easily.

I’ll admit it—I let it get to me. I started wondering if what I write even makes a difference. If anyone really reads these little dispatches from the caregiving trenches, or if I’m just yelling into the void with spellcheck.
Then I talk to many of you. I hear your stories. I see the “me too” and the “I thought I was the only one” and the “thank you for saying it out loud.” And just like that, I remember why this matters.
So… it’s time to saddle up and ride again.
There are literally millions of us doing this work—quietly, daily, relentlessly—trying to figure out a path that doesn’t come with a map. And we’re all saying versions of the same sentence:
This is hard.
Not “cute hard.” Not “busy season hard.” This is soul-sucking, identity-blurring, never-clock-out hard. And also… somehow… it’s blessed. Not because it feels shiny. But because love is stitched into it. Because showing up matters. Because honoring someone—especially when it’s messy and unglamorous—has weight.
I’m a Christian, and I’ll tell you plainly: my faith is what holds me up when my nerves are fried and my heart is tired. Additionally, there is my daughter who reminds me I have other roles in this life. My mother (yes, you read that right—sometimes she is the one who grounds me). And my little animals, who have never once asked me a repetitive question, but have absolutely judged me for crying while holding a cheese stick and not sharing.
Here’s the magic recipe, and it’s annoyingly simple:
We are all doing the very best that we can – and that’s the sum of it.
There are no rules. No one-size-fits-all handbook. No gold medal for “most put-together caregiver.” Some days the win is brushing your hair. Some days the win is keeping your mouth shut. Some days the win is not running away to live on an island where nobody needs a snack, an explanation, or your last nerve.
Screaming in cornfields is normal.
Crying in the pantry is not only valid—it’s basically a rite of passage. And gummy bears? Honestly, they’ve earned a place in the caregiver tool kit.
This life we’re living doesn’t always sparkle. But it’s sacred.
It’s holy ground wrapped in mismatched socks and pill bottles. It’s early morning tears and late-night numbing. It’s loving someone fiercely while grieving who they used to be—and sometimes grieving who you used to be too.
But here’s the part we forget, and I want to say it like I’m looking you dead in the eye:
You are still here.
You still matter.
Even if your life feels paused, your purpose isn’t. There is purpose.
If my brain feels a little jumbled this morning… just roll with me. That’s kind of the brand around here anyway.
Faithful, Not Flawless
God isn’t asking you to be a martyr—just to be faithful. If you want to find proof of that, look for the story of Hagar in Genesis. It’s an eye opener – she’s a caregiver of another sort, but she knew without a doubt that God saw her. He sees us too. It’s the one time in the bible that he is called by the name El Roi. If you want to know more, just ask.
Faithfulness doesn’t mean perfection. It means showing up with bedhead and broken patience. It means apologizing when you snap. It means honoring your limits instead of bulldozing right through them like you’re invincible (spoiler: you’re not, and neither am I).
You’re allowed to be tired. You’re allowed to be mad. And you are absolutely allowed to ignore people who have no clue what this life actually demands. Maybe they BELIEVE they are being helpful – or perhaps they are the true reincarnation of the Mother Theresa (kidding – they aren’t).
So no, I haven’t written in a while – but here I am – bedhead fire and all.
You’re not alone.
We’ll keep supporting each other, laughing and crying together – even if some days it feels like we’re crawling on our elbows.
You’ve got this. And if you don’t? That’s okay. I’ll hold the line until you can. No hacks this week, just care, and understanding.